“So, what brings you in today?”
The young Filipino lady before me wrung her thin hands together. Her eyes betrayed a sense of fatigue as the corners of her eyes crinkled with anxiety. “Doctor, I am still feeling dizzy.”
Dizziness is a common complaint, but a difficult one to get a handle on. So many different things manifest themselves as dizziness… an unsteadiness with walking, the presyncopal feeling like you are going to pass out or just the sensation of violent spinning (the same as how you felt as a child after twirling in circles in the park or on an office chair). “What do you mean?”
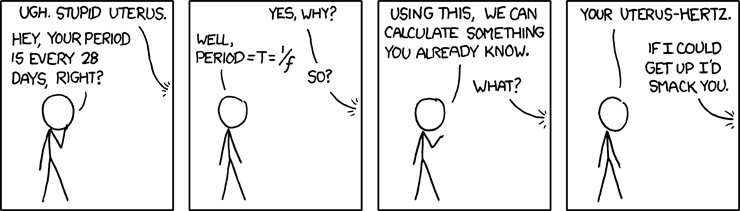
“Well, it started almost two months ago. I had two episodes of dizziness that went on throughout the day that lasted for a few seconds. It felt like I was spinning in a circle. I was worried so I went online to see what could cause it. And I tried to make an appointment with my family physician but that would be in a few weeks so I saw an audiologist, a neurologist and a psychiatrist too. The audiologist tested me for nystagmus and had me perform the Dix-Hallpike maneuvers and asked me if I was dizzy. I told her no, but she noted some eye movements with the electronystagmogram so she diagnosed me with bilateral benign paroxysmal positional vertigo anyway. She prescribed some modified Epley maneuvers. The neurologist thought I might have migraine-related vertigo and put me on Amitryptyline. And this whole time I was doing research online I would read about these different symptoms and I would start to get them! My parents were very worried and suggested that I see a psychiatrist for my anxiety. He put me on Sertraline and Clonazepam.
Wow… I thought to myself. That’s quite a few specialists! This was a highly educated woman… she understood what nystagmus and Epley maneuvers were, and she could pronounce BPPV which put her pretty much at my level as far as I was concerned. Yet after seeing all of these different doctors, she was still here in the FM clinic even though her last visit was *flips through the chart* two weeks ago… when she was given meclizine for nausea.“Uhm, I’m sorry…” I apologized. “I don’t understand. You’ve been diagnosed with BPPV and anxiety with the possibility of migraine-related vertigo… what can I do for you today?”
“I just want help. I am not feeling the spinning dizziness anymore. That was a long time ago. Now it is more of a… it’s hard to describe. It’s a rocking sensation.” “Like you’re on a boat?” I offered. “Sort of.”
It took me a while to piece the whole story together, but it seemed like her main complaint of dizziness had resolved but she was having residual anxiety and a number of other unusual symptoms -- getting visually overwhelmed by venetian blinds and patterns on carpets and being unable to go into a store without feeling anxious. However, she persisted on calling it dizziness with her subsequent physicians, although perhaps “uneasiness” would be a better way to put it. She told me that when she saw the audiologist and the neurologist, she was feeling very anxious about what was going on… but aside from performing tests like an ENG and an MRI of her head, they offered little comfort or support except to say “Go see your family physician.” She saw the psychiatrist about a week ago and after some persistent questioning about functioning, she said that she felt much better with the SSRI and benzodiazepine.
While I do not doubt the technical ability of the audiologist to interpret an ENG or a neurologist’s ability to identify and treat a migraine headache, these skills have their time and place. Her underlying problem was the anxiety she was having about the dizziness which took over and became a general sense of worry and unease. These specialists were ill-equipped to deal with that aspect -- and it was not until the Family Medicine doctor intervened that the whole picture could be assembled for the patient.“You’ve seen a number of specialists and they have helped us rule out dangerous things like a brain tumor. You are still able to work and you have not had any difficulty walking, so functionally you’re doing really well. I understand that you’re feeling dizzy. The good news is that it is nothing serious as far as we can tell so far!” She left feeling reassured and I saw her with the psychiatrist as well to keep up the continuity of care.
The culture of medicine has changed and I feel that this is the crux of it! This patient had fallen through the cracks of the system. She tried to get an appointment with her PCP and when she couldn’t see her immediately, she resorted to a series of more expensive but ultimately unfulfilling specialists before her family helped her find someone address the underlying problem. She needed someone to put the pieces of the puzzle together. All too often, patients think that specialists are better than primary care for everything and this fragmentation of care leaves the patients with the pieces. Even worse, they assume that their primary care physician is automatically receiving all of these specialist reports! It is hard to piece all of these things together from a confused patient. I think that family medicine physicians are more than care coordinators or a bouncer at the specialty doorway. Similarly, specialists are more than just procedural technicians who punt back even small things like reassurance and education back to a family physician. All doctors go to medical school instead of OR or ER or psych ward school for a reason. We all know the basics of patient care.
A recent
New Yorker article by Atul Gawande, entitled the “Cost Conundrum” also addresses this “Culture of Medicine.” Gawande outlines the problem of controlling health care costs by comparing the habits of physicians living in McAllen, Texas to nearby El Paso, Texas. He also went to Mayo clinic in Rochester, Minnesota, where he expected that their world-wide renown, high-tech and high quality of care would equate to more money.
McAllen’s Medicare expenditures per enrollee in 2006 were $15,000.
El Paso’s were $7,500.
Mayo clinic's were $6,688, less than either McAllen or El Paso!
What accounted for this difference?
McAllen physicians were highly enterprising and saw more patients each day, ordered more tests, and performed more aggressive interventions earlier. This padded their pockets a little bit more and thus rewarded, they continued onwards. This cycle of greed and profit is perfectly legitimate in our system of Relative Value Units (RVUs) where procedures are valued above cognition and doctors are compensated not be the quality of their patients’ health or their ability to make a diagnosis in a cost-effective manner… they are paid based on how many patients they see each day. This drives them to maximize their patient numbers and minimize their time with each of them! It becomes much easier to check a box and order an MRI of the brain than it is to spend an extra TEN minutes with a patient to sort out the true history and duration of dizziness -- but which one is more ideal?
I think that healthcare will be the next bubble to burst, now that dot.coms, real-estate markets, Wall Street and Auto makers collapsed under similarly empty value-for-cost pressures. Our healthcare dollars are being poured down a hole with little regard about whether they are spent on the RIGHT things. Gawande made a comment that I found
Twitter-worthy:
“the most expensive equipment is a doctor’s pen. And, as a rule, hospital executives don’t own the pen caps. Doctors do.”
The culture of medicine needs to change if we are going to fix our “broken system." Doctors cannot sit idly by and complain that it is insurance reimbursement or Medicare that is causing the problem. We need to admit that
we are a part of the problem -- and seeing patients as a revenue stream and maximizing “business” by turning up the speed on the conveyor belt is
not the solution! There is a sense of entitlement that because we have worked so hard and studied for so long to get to the position that we are in today (or in my case, soon will be,) we deserve the highest compensation for our services as possible. We measure our success based on how our income and lifestyle compares to our peers -- and so, in medical school, ironically fields like anesthesiology and radiology are highly valued despite the minimal patient contact. (It's a
a pissing contest, if you pardon my French.) Our value to society and our true measure of success should be based on how healthy we keep our patients and how comfortable we make them feel when we cannot. That's our value to keep healthcare costs down!
We do not gain the sympathy of the general public by complaining -- “I don’t get paid enough to see patients!” Many patients who go to the doctors only to find a nurse practitioner or a physician assistant may just reply -- “You never saw me anyway.” We need to ground ourselves again and remember that our duty is to Care for patients before ourselves. That’s my interpretation of the words “Primary Care.” And that’s Not My Second Opinion!












![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=29c0e8e4-bb2d-4b1f-a0ad-cfe84a3b9f7c)



